Family Planning and Newborn Survival: Diminishing Returns
Improved child survival is one of the major global health goals, and for good reason. Not only are many deaths of newborns, infants, and children the result of preventable or treatable causes, but also they are concentrated in areas of greatest poverty and deficits of health care infrastructure. Globally, the huge disparities between child mortality rates between countries and regions indicate that solutions exist, but are not distributed evenly.
There are different ways to look at reducing child mortality. One way is to talk about reducing the number of deaths in total; another way is to discuss reducing the rate at which deaths occur. The number of deaths gives an indication of the burden of child mortality, but this is impacted by the size of the population: if there are two countries with similar child survival rates, but one has a larger population, the number of deaths in that country will be greater even if the risk to any one child is not. In contrast, the child mortality rate, which is typically calculated as the number of child deaths per 1,000 live births, gives an indication of the risk of death in a given region, without reference to population size or fertility rates in that region.
If the goal is to reduce child mortality by making childhood safer, then the more useful measurement is the child mortality rate. If, however, the goal is to advocate for reduced fertility under the banner of child survival, the key figure is the number of child deaths. After all, you can reduce that number by ensuring more children survive…or by ensuring that fewer children are born.
I’ve written about the way family planning advocates sometimes spin child lives averted by contraception as “lives saved” by a sort of therapeutic nonexistence—it’s also a major problem in a piece of currently-pending legislation in U.S. Congress known as the Reach Every Mother and Child Act (REACH Act).
But there is another interesting aspect of this issue, which is the tension that exists between the two types of child mortality measurements. In short, the more we improve child outcomes by scaling up the types of interventions that actually leave child survivors, the less traction the “averting deaths by averting lives” argument actually has.
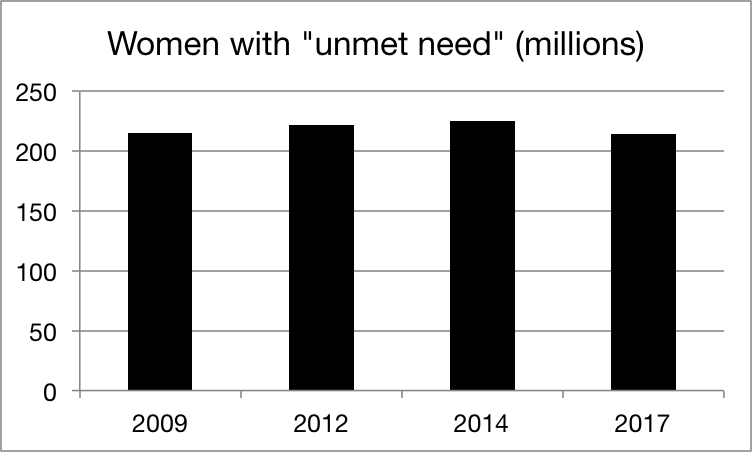
Every few years, the Guttmacher Institute releases a report called “Adding It Up,” (AIU) which makes the case for increased spending on family planning in global health. One of its key metrics is the so-called “unmet need” for family planning—which should not be confused with lack of access or actual demand for the same. A look at the last several AIU reports reveals that, on the whole, the number of women being characterized as having an “unmet need” has held relatively constant:
Many of the claims Guttmacher makes in the report center around the hypothetical outcomes of meeting the entire “unmet need.” Setting aside the obvious problem that doing so would necessarily involve convincing millions of women to set aside their health concerns, religious views, and personal opinions in a variety of ways, let’s assume for the sake of argument that we could somehow turn each of those women into a modern-contraceptive user. This would presumably result in a reduction in births to those women; AIU’s estimates are here:

Again, not much difference across the years, which corresponds to the previous figure. But what about the promise of reduced infant mortality? AIU also gives estimates for the number of infant deaths (that is, deaths under one year of age) that would potentially be averted by meeting the entire “unmet need”:

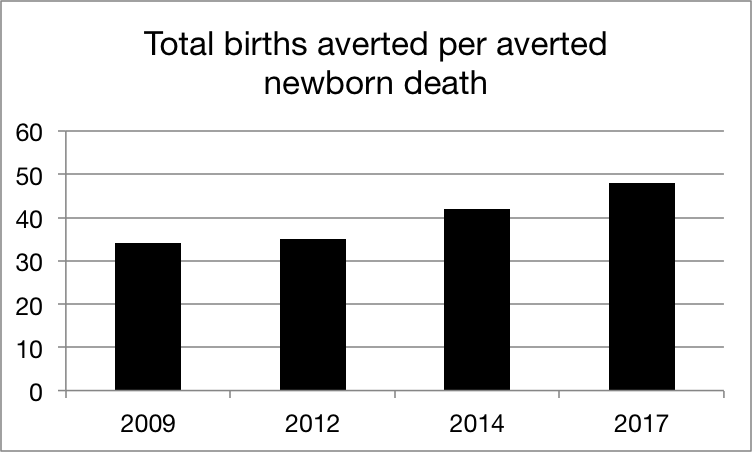
From 2009 to 2017, we see a 25% reduction in the number of projected averted deaths, as compared to just a 5% reduction in the number of projected averted births. Why would that be? The answer is in reductions to the infant mortality rate, or the number of infant deaths per 1,000 live births. As infant survival improves due to overall improved health care, the risk of death to the average infant goes down. Or, to put it another way, you have to avert more births to avert a diminishing number of infant deaths:
It could be argued that the reduction in infant deaths may be due in part to improvements in birth spacing, in turn due to increased contraceptive use. Demographers have hypothesized that increased knowledge of family planning can in fact increase “unmet need” as women who are unaware that methods exist will not be in a position to demand them. However, survey data indicate that knowledge of family planning methods is now near-universal. As for the birth spacing argument, while it makes for an interesting discussion, it’s notable that most attempts to estimate infant or child deaths averted by contraceptive use rely on a demographic model that does not differentiate between low- and high-risk pregnancies.
(As a side note, AIU also includes estimates of averted maternal deaths by meeting the entire “unmet need,” but due to significant changes in the calculation of maternal mortality during this same period of time, the numbers are unlikely to be comparable.)
Taken together, Guttmacher’s estimates over the years paint a picture of diminishing returns when it comes to contraceptives and infant survival. While fewer births may mean fewer deaths, this is hardly a useful public health argument: taken to its logical conclusion, one might as well argue that contraception is the single most cost-effective way to prevent deaths from cancer or Alzheimer’s disease, since fewer older people would mean fewer cases of both, regardless of improved treatments for either.
Family planning advocates have been incredibly adept at framing their single solution as the fix for a variety of societal problems, ranging from maternal and child health to women’s empowerment to environmental issues to economic growth. As progress is made in tackling some of the world’s toughest epidemics, the World Health Organization and the UN have turned their attention increasingly to noncommunicable diseases (NCDs)—predictably the “sexual and reproductive health and rights” crowd are following the buzz…and the money.
Ultimately, what counts is what gets counted: choose the wrong measurement of success, and you will choose the wrong solutions to achieve it. If powerful players in the global health arena buy into the notion that nonexistence is a form of health care, the only ones to benefit will be the advocacy groups who argue that it is possible to contracept your way to improved infant survival.
View online at: https://c-fam.org/turtle_bay/family-planning-newborn-survival-diminishing-returns/
© 2024 C-Fam (Center for Family & Human Rights).
Permission granted for unlimited use. Credit required.
www.c-fam.org

